Patient Self-Management Credentialing and Value-Based Health Benefits Design Considerations in Patient-Centered Team-Based Care
Introduction
Patient credentialing is a unique concept where the patient’s knowledge, skills, and performance associated with their chronic disease, lifestyle requirements, and therapy adherence strategies are assessed so health care providers can tailor education, support and care that effectively meets the specific needs of individual patients. The Patient Self-Management Credential (PSMC) is a psychometrically validated care resource that empowers health care providers and patients to work together in meaningful and efficient ways to identify and address areas for improvement in the self-management of health. With a progressive evidence-base that has evolved over the past 14 years, use of the PSMC has consistently produced patients that are more engaged and empowered to manage their own health care.
Convening a Consortium of Key Stakeholders
The APhA Foundation convened a consortium to further explore challenges within the current healthcare system as well as opportunities for potential system changes. The consortium provided insights and principles that could be used to guide institutions in making value-based health benefit decisions.
Perspectives from four key constituencies were considered:
1) patients who have been empowered by their providers through use of the PSMC,
2) practitioners who have utilized the PSMC in their practices to customize care,
3) payors who make data-driven decisions to inform their coverage, and
4) value-based health decision makers from benefit managers and health systems.
Recommendations from Consortium
A synthesis of the information, opinions, and expertise that emerged from the Consortium discussion produced six key themes that provided the basis for developing a principle-centered approach that will contribute to optimizing health and costs of care.
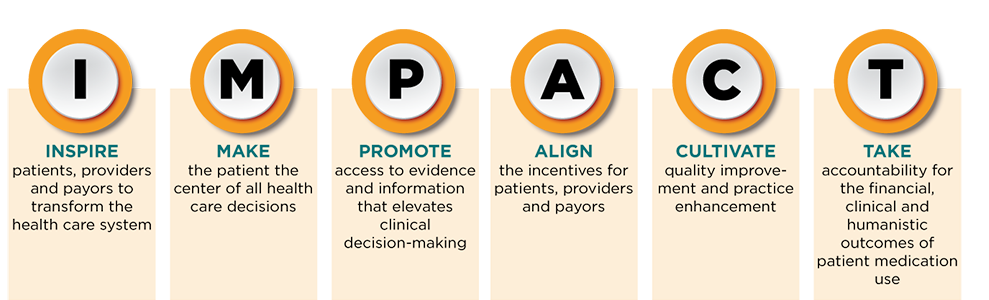
The Key Principles for Transforming the Delivery of Patient Care that could IMPACT effective health care system changes and improve patient outcomes are to:
Inspire patients, providers and payors to transform the health care system
Make the patient the center of all health care decisions
Promote access to evidence and information that elevates clinical decision-making
Align the incentives for patients, providers and payors
Cultivate quality improvement and practice enhancement
Take accountability for the financial, clinical and humanistic outcomes of patient medication use
The APhA Foundation will continue to work with system stakeholders to develop tools and resources that will guide stakeholders on “how” to translate these principles into practice and invent a preferred future for our health care delivery system.
|
Expert Panel Participants |
||
|
Name |
Title |
Organization/Affiliation |
|
Amanda Applegate |
Pharmacy Clinical Services Coordinator |
Balls Food Stores |
|
Tery Baskin |
President and CEO |
RxResults |
|
John Beckner |
Senior Director, Strategic Initiatives |
National Community Pharmacists Association |
|
Dean Benton |
Clinical Coordinator |
Dillons Pharmacy |
|
Benjamin Bluml |
Senior Vice President, Research and Innovation |
APhA Foundation |
|
Kelly A. Brock |
President |
KB Pharmacy Solutions |
|
Barry Bunting |
National Practice Leader, Health Plan Innovation |
Ateb |
|
Mark Cziraky |
Vice President of Research |
HealthCore, Inc., an Anthem Company |
|
John Forbes |
Owner |
Medicap Pharmacy |
|
Scott Hamstra |
Infectious Disease Specialist |
U.S. Indian Health Service |
|
Elizabeth K. Keyes |
Executive Director |
APhA Foundation |
|
Sandra Leal |
Vice President for Innovation |
SinfoniaRx |
|
Thomas Menighan |
Executive Vice President and CEO |
APhA |
|
Shannon Peter |
Clinical Pharmacy Manager |
Think Whole Person Healthcare |
|
Pete Sheldon |
Vice President, Education & Patient Engagement |
Med-IQ |
|
Steve Simenson |
Managing Partner |
Goodrich Pharmacies |
|
Jaan B. Skelton |
President |
Silver Pennies Consulting |
|
Parisa Vatanka |
Project Development Manager |
APhA Foundation |