We begin with the end goal in mind – to improve healthcare.
Our Research Process
Our research explores and evaluates innovative models of care that enhance healthcare quality by integrating pharmacists into the healthcare team.
Our Focus:
- Empower patients
- Increase collaboration between pharmacists, physicians and other members of the healthcare team
- Enhance safety through optimization of medication use
- Align incentives for patients, providers, and payers
- Improve health outcomes
- Reduce healthcare costs
Innovation Arc
The APhA Foundation’s Innovation Arc, pictured to the right, depicts the types of transformative work that has been conducted since the late 1990s. Our work on a specific topic can begin anywhere along this spectrum then evolve and grow.
The Innovation Arc includes:
- Convening thought leaders to explore ideas for new areas of pharmacy practice
- Developing a model and testing it in a pilot project
- Refining the model based on learning from the pilot and scaling the work into more areas and populations
- Continually improving the model so its success can be nationally implemented to impact healthcare all across America.
See our work on diabetes to see the innovation arc in action.
How the Model Works
How the Model Works
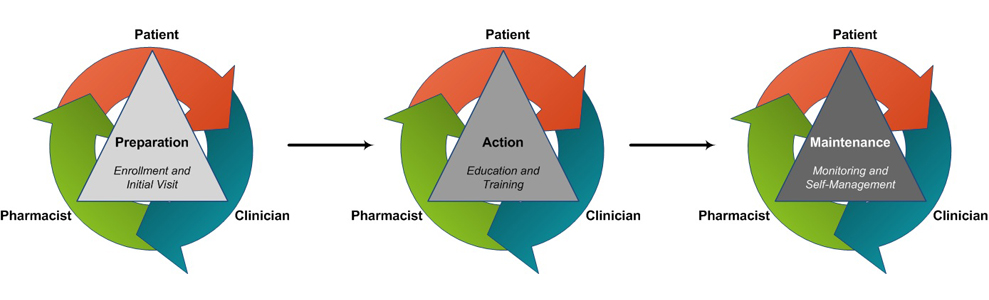
Many of the APhA Foundation’s practice-based research initiatives are developed from a proven process model in which patients, primary care providers, pharmacists, and other health care professionals work together to empower patients to be effective self-managers of their health. This care model includes pharmacist coaching and interventions related to medication therapy, lifestyle modifications, and ongoing chronic disease monitoring. The pharmacists and providers share an open line for bi-directional communication and collaborate with their patients to set and achieve realistic health goals. The process of care model is segmented into three areas as the patient moves along the spectrum of disease control.
- Preparation: Patients are enrolled in the project by physician-, pharmacist-, or self-referral The patient completes a medication history form and informed consent, and the pharmacist engages with the patient during a first visit. The pharmacist uses motivational interviewing and point-of-care testing to gain an understanding of the patient’s health condition, chronic disease control, and current care plan. The pharmacist, patient, and other providers work together to develop a plan for optimizing the patient’s care.
- Action: During subsequent visits with the pharmacist, patients receive education and training that is tailored to meet individual needs related to monitoring and controlling their conditions. Pharmacists work with other providers to share information, update treatment goals, and reinforce action steps from the care plan. The Action phase may last the patient’s entire lifetime, as they continually work with the healthcare team to improve their health.
- Maintenance: Once the impact of effective self-management is realized, the Maintenance phase allows for ongoing monitoring of the patient’s health through as-needed check-ups with the pharmacist and other members of the healthcare team. Involvement in the Maintenance phase assures that patients remain accountable for continuing self-management behaviors and identify areas for Action as they arise.
Collaboration is the cornerstone of the success of this model. Pharmacists are a healthcare solution and can dramatically help to improve patient outcomes when integrated into healthcare teams. The APhA Foundation’s approach is to continuously search for and evaluate the next innovation that will improve people’s health through pharmacists’ patient care services.
CTA - PSMS
Explore how to implement our approach with your patients or beneficiaries.